Medical Professionals Who Have Disabilities: Why I Like to Help
By Cassie Springer Ayeni
I’ve developed a bit of a niche within my specialization of employee benefits (ERISA) law: I have helped numerous medical professionals secure their partial or complete disability benefits. My clients have been OBGYNs, family medicine practitioners, physical therapists, PICU M.D.s, gastroenterologists, specialized nurses, and more. I wonder: do I gravitate to them or do they gravitate to me?
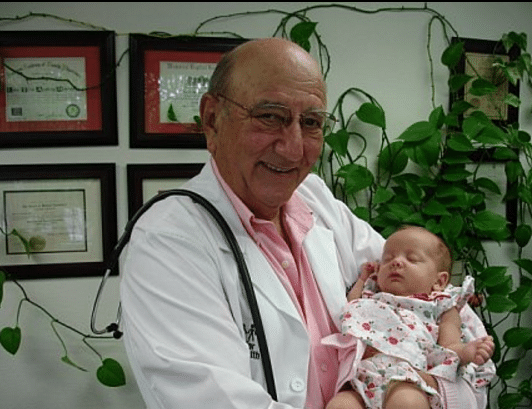
I’ve always been a money saver, and to further that goal I started working during summers and after school when I was 13 years old. One of my favorite teen jobs was in the file room of my father’s medical office. I would take slips of dictation and put them into the right patient’s file, skimming the details and, without knowing it, becoming familiar with medical terminology and the fascinating process of diagnosis. I loved reading the symptoms, findings, and conclusion that came from every interaction and examination. I got a lot of paper cuts, but I also learned early lessons in medical analysis and interpretation.
My father is one of a dying breed in the world of medicine: a jack of all trades. He’s a family practitioner, and in the 1970s he even used to deliver babies. He performs and assists on surgeries, sees people of all ages, and is loved by his patients. I am the middle child of the 6 he fathered, and he once told me he thought I would take over his practice someday. But I excelled in writing, not chemistry, and my passion for analysis fell to the pages of Jane Austen and later Supreme Court cases, not to Gray’s Anatomy.
Yet here I am, 15 years into a career that involves reading and interpreting medical records every day, just as I did in my father’s office so many years ago. This time, though, I am reading these records for evidence in support of my client’s employee benefits disability claim against an insurer. I have read through hundreds of thousands of pages of medical records in my career, MRIs, CT Scans, labs and more, figuring out medical shorthand along the way, to make arguments to insurance companies and courts about why the medical evidence demonstrates a lack of work capacity.
Maybe it’s this familiarity with the tools of the trade that has resulted in a plethora of medical professionals as clients: I respect their craft and understand the tip of the iceberg, so I am particularly eager to help these clients out when a disability causes them to cut back their duties or stop working altogether. Whatever the reason, I certainly enjoy representing doctors and nurses, and I feel so fulfilled when one of my medical professional clients recommends a colleague connected to her/him. And by the way, my father is 75 years old and still working nearly full-time as a physician. Life Goals.
Cassie Springer Ayeni is the President of Springer Ayeni, A Professional Law Corporation, in Oakland and San Jose, California. She focuses on representing people in ERISA disability and life insurance cases. She can be reached at cassie@benefitslaw.com or www.benefitslaw.com
Read More
Reforming Disability Claim Procedures Under ERISA
On Dec. 19, 2016, the U.S. Department of Labor published in the Federal Register sweeping reforms to the regulations it issues under Section 503 of the Employee Retirement Income Security Act, aimed at eliminating bias in the ERISA disability claims and review process.
Despite ERISA’s reputation as an erudite law affecting primarily pension plans, the DOL reports that, “An empirical study of ERISA employee benefits litigation from 2006 to 2010 concluded that cases involving long-term disability claims accounted for 64.5 percent of benefits litigation whereas lawsuits involving health care plans and pension plans accounted for only 14.4 percent and 9.3 percent, respectively.” (p. 3.) Hence the DOL’s decision to take aim at the regulations affecting disability plan administration, which is typically handled by insurance carriers.
The DOL noted “the economic incentive for insurance companies to deny otherwise valid claims and because plans are often able to secure a deferential standard of review in court.” (p. 8.) Although the DOL received commentary that disability claims administrators should not be subject to the same rigorous regulations issued under the Affordable Care Act to health plan administrators, “the department views enhancements in procedural safeguards and protections similar to those required for group health plans under the Affordable Care Act as being just as important, if not more important, in the case of claims for disability benefits.” (p. 10.) It noted the need for transparency and accountability in all claims handling. (p. 11.)
The department enhanced protections for disability plan participants in eight ways (pp. 11-12):
Increased independence and impartiality of the decision makers
Adverse decisions must fully explain the reasons for the denials and why evidence of the claimant was disagreed with
Notification to claimants of the right to obtain their claim file and other documents before a final decision is made and to present testimony and other evidence in support of their claim
Provision of an opportunity for claimants to respond to adverse medical opinions before a final decision is made
A guarantee that a claimant can proceed to litigation if the administrator fails to comply with the DOL regulations (stricter than “substantial compliance”)
A guarantee that a rescission of coverage triggers appeal rights under the regulations
Cultural and linguistically appropriate requirements for communications
A requirement that the notice of an adverse benefit determination on review must include a description of any applicable contractual limitations period and its expiration date (p. 54)
But perhaps the biggest protection is the first, requiring impartiality not just in claims decision makers, but also in vocational experts, medical consultants and in-house medical reviewers. (pp. 13-15.) And the DOL understood and took issue with the notion that impartiality could be achieved if the administrator, for example, hires a company who then hires the medical expert for review. It stated: “The text of the rule does not limit its scope to individuals that the plan directly hires. Rather, the rule’s coverage extends to individuals hired or compensated by third parties engaged by the plan with respect to claims.” (p. 15.) It cautioned that such a prohibition should not temper a court’s inquiry into the neutrality of the expert, noting the availability of discovery to probe such matters. (p. 16.)
The DOL further disabused the insurance practice of rejecting experts that would support an approval of benefits in favor or experts that would support denial as inappropriate “expert shopping.” (p. 20.) It found that “[r]equiring plans to explain the basis for disagreeing with experts whose advice the plan sought” should help that problem. (p. 20.) The department couched the requirement to explain disagreement with medical and vocational professionals in denying a claim “as a matter of basic fiduciary accountability.” (p. 22.)
Regarding Social Security disability awards, the department was careful to specify that although it does not expect administrators to defer to a favorable Social Security disability determination, “a more detailed justification would be required in a case where the U.S. Social Security Administration definitions were functionally equivalent to those under the plan.” (p. 25.) It refused, however, to adopt the “treating physician rule” present in Social Security decisions, where the administrator must defer to the opinion of the treating physician. (p. 25.)
The department vigorously defended its decision to allow claimants to review and rebut evidence that would be used to deny a claim. Commenters argued that claimants could provide an endless loop of evidence supporting a claim that the administrator would have to rebut endlessly as well. The DOL dismissed that argument as contrary to fiduciary obligations: “The fiduciary obligation to pay benefits in accordance with the terms of the plan does not require a fiduciary to endlessly rebut credible evidence supplied by a claimant that, if accepted, would be sufficient to justify granting the claim. In fact, an aggressive claims-processing practice of routinely rejecting or seeking to undermine credible evidence supplied by a claimant raises questions about whether a fiduciary, especially one operating under a conflict of interest, is violating the fiduciary’s loyalty obligation under ERISA to act solely in the interest of the plan’s participants and beneficiaries.” (p. 37.)
Controversially, the department approved a “tolling” of timelines for responding to claims and appeals where the claimant submits additional evidence for the administrator to consider. “In the department’s view, the current disability claims regulation ‘special circumstances’ provision permits the extension and tolling expressly added to the group health plan rule under the ACA claims and appeals final rule.” (p. 40.) It remains to be seen if this will deny claimants swift access to the courts or even allow a statute of limitations to expire while tolling is in place. See Heimeshoff v. Hartford Life & Accident Insurance Co., 134 S.Ct. 604, 611 (2013). Perhaps in anticipation of this conundrum, the department addressed the potential problem raised by the Heimeshoff decision where a statute of limitations could expire while a participant was engaging in the mandatory review process prescribed under ERISA Section 503. It stated:
First, Section 503 of ERISA requires that a plan afford a reasonable opportunity to any participant whose claim for benefits has been denied for a full and fair review of that decision by 53 an appropriate named fiduciary. The department does not believe that a claims procedure would satisfy the statutory requirement if the plan included a contractual limitations period that expired before the review was concluded …
A limitations period that expires before the conclusion of the plan’s internal appeals process on its face violates ERISA Section 503’s requirement of a full and fair review process. A process that effectively requires the claimant to forego the right to judicial review and thereby insulates the administrator from impartial judicial review falls far short of the statutory fairness standard and undermines the claims administrator’s incentives to decide claims correctly. (pp. 52-53.)
It further stated that a contractual limitations period that does not permit a lawsuit after the conclusion of an administrative appeal “is unenforceable.” (pp. 53-54.) In an effort to provide transparency, the department will now require administrators to state any contractual limitations period “including the date by which the claimant must bring a lawsuit” in a final adverse decision. (p. 53.)
However, the department did not provide much leeway for plan administrators to avoid litigation for failing to comply with the regulations. In fact, for the administrator to argue failure to exhaust administrative remedies despite noncompliance, the administrator’s failure to comply must be all of the following: “(1) de minimis; (2) nonprejudicial; (3) attributable to good cause or matters beyond the plan’s control; (4) in the context of an ongoing good-faith exchange of information; and (5) not reflective of a pattern or practice of noncompliance.” (p. 42.)
The department refused to provide a general rule on the level of deference an administrator would receive from a reviewing court, but did indicate that where the administrator’s noncompliance has resulted in a claim’s deemed exhaustion, the “legal effect of the definition may be that a court would conclude that de novo review is appropriate because of the regulation that determines as a matter of law that no fiduciary discretion was exercised in denying the claim.” (pp. 43-44.)
Read More
At What Stage of an ERISA Disability Claim Should You Retain an Attorney?
By Cassie Springer Ayeni; cassie@benefitslaw.com; www.benefitslaw.com
Today I met with a client who was in a pickle — she had already applied for disability benefits and was feeling nervous and pressured by an insurance company to provide additional information when she thought she had already submitted everything. Her question: should I hire you now or later? When it comes to ERISA disability claims, often the sooner you hire an attorney, the better.
Sure, most attorneys make more money if you’ve gone through the denial and appeal process on your own. After all, attorney fees skyrocket once you’re in litigation. Therefore they might encourage you to apply on your own then come back after you have a denied benefit to be appealed or litigated. But is this really in the client’s best interest? I think not. Indeed, I think attorneys have an ethical duty to try to obtain a favorable decision as soon as possible because that is in the client’s best interest.
But what advantage can an ERISA attorney provide when it’s just a submission of a claim application? An attorney worth her salt will not simply oversee form submission when it comes to applying for disability benefits. Rather, she will not only make sure that the forms are completed correctly, but she will anticipate future insurance company questions and submit supporting documentation before the insurance company asks for it. A complete claim submission packet can be almost as thick as an appeal of a denied benefit claim, containing medical evidence, analysis, sworn statements, and much more.
Although it is best to involve an attorney at the application stage, it does not occur to most people to do so until after a claim has been denied. This is OK too! However, for an attorney to do a great (not just good) job appealing a denial, that attorney must invest substantial time into obtaining all of the medical evidence necessary to prove your case and rebut the insurance company’s position. Why? Because if you have to sue the insurer in federal district court to obtain your disability benefit, under ERISA the judge is typically limited to reviewing only the medical evidence that appears in the claim and appeal record. In other words, there is no second chance to prove your case from a medical perspective once you file a lawsuit. Therefore, it is crucial that an attorney well-versed in ERISA does a great job with your appeal. A half-baked appeal or a submission of evidence without analysis will rarely get a favorable result.
The lesson is: when it comes to ERISA disability cases, the earlier you seek guidance from an ERISA attorney, the better. As for the potential client today? I gave her the same advice: 1) she could retain me to halt the application she submitted and to supplement with all of the additional documents I know she needs to succeed; or 2) she could roll the dice and see if she prevails (medically, she definitely should be entitled to benefits!). But with option 2, ultimately it takes more time and resources to reverse a denial than it takes to do it right the first time.
Read More
PRACTICE GUIDE: ERISA ISSUE SPOTTING – HOW TO AVOID MALPRACTICE
ERISA. The acronym strikes terror in the heart of many a lawyer. Fuzzy notions of fiduciary duties, equitable remedies in the days of a divided bench, and preemption can cause even the most erudite of attorneys to break into a cold sweat. My friends: speaking as someone who has handled ERISA claims, litigation, and appeals for 15 years, I’m here to tell you that it is really not that bad! Allow me to walk you through some ERISA basics so that you can issue spot and avoid malpractice.
ERISA Fundamentals
The Employee Retirement Income Security Act of 1974 (ERISA) provides minimum standards for voluntarily established benefit plans in the private industry. In addition to pension plans, ERISA governs health and welfare benefit plans, including employer-sponsored disability and life insurance plans. ERISA does not cover benefit plans established or maintained by governmental entities, churches for their employees, or plans which are maintained solely to comply with applicable workers compensation, unemployment, or disability laws. This means that UC plans are non-ERISA (government) plans, but an employer’s benefit plans are governed by ERISA.
ERISA requires plans to provide participants with plan information. ERISA § 104(b)(4). Those who manage and control plan assets must act as fiduciaries. ERISA § 404. ERISA plans must have a grievance and appeals process for benefit claims. ERISA § 503. The process of appealing a denied benefit claim is also called a “request for review,” and is crucial to achieving success on a denied benefit claim, either with the administrator or before a federal court. TIP: There is a 180-day deadline for submitting ERISA appeals that CANNOT be missed. Finally, ERISA gives participants and beneficiaries the right to sue for benefits and breaches of fiduciary duty. ERISA § 502(a). Lawsuits related to or remedied by ERISA are brought in federal district court. Statutes of limitations are often identified in the ERISA plans themselves and must be adhered to.
ERISA Preemption
ERISA has broad preemption provisions. ERISA § 514. If a remedy is available under ERISA, the claim will be preempted. If a case “relates to” an ERISA plan because there is a “connection with or reference to” a plan, the case will be preempted. Metro. Life Ins. Co. v. Massachusetts, 471 U.S. 724, 739. For example, in Ingersoll-Rand Co. v McClendon, the Supreme Court held that a wrongful discharge action was preempted by ERISA because the plaintiff alleged that the wrongful termination was primarily because of the employer’s desire “to avoid contributing to, or paying benefits under, the employee’s pension fund.” 498 U.S. 478, 483 (1990). However, in another case, the Supreme Court determined that California’s prevailing wage law is not preempted by ERISA because the law does not “make reference to” ERISA plans, nor does it have a connection to an ERISA plan because “[t]he prevailing wage statute alters the incentives, but does not dictate the choices, facing ERISA plans.” California Div. of Labor Standards Enf’t v. Dillingham Const., N.A., Inc., 519 U.S. 316, 328, 334 (1997).
As a general rule, if the alleged harm is that the unlawful conduct interfered with a right to receive, vest in, or accrue an employee benefit, then the claim will be preempted. Ingersoll-Rand Co. v. McClendon, 498 U.S. 133 (1990) (preempting a common law wrongful discharge claim where the claim was that the employer retaliated to prevent vesting in an ERISA plan). TIP: If you are concerned that your case will be pre-empted by ERISA, avoid alleging that any remedies are available under any kind of employee benefit plan or that any claims bear a connection to an employee benefit plan. Do NOT allege that the bad behavior caused a loss of employee benefits. Do NOT allege that the bad behavior should result in payment of disability or other ERISA benefits. These allegations will cause you to be removed to the federal courts that have exclusive jurisdiction over ERISA claims. And, if the claim is properly an ERISA claim for benefits, then there will be no consequential or punitive damages available, nor will there be a jury trial.
However, ERISA’s “savings clause” provision saves from preemption any law that regulates insurance, banking, or securities. ERISA § 514(b)(2)(A). An example of the application of the savings clause is in California’s “notice prejudice” rule, which provides that claims can proceed even where there is late notice unless the insurer is prejudiced by the late notice. Because this is a law that regulates insurance and does not provide a remedy that conflicts with ERISA, the law is not preempted. UNUM Life Ins. Co. of Am. v. Ward, 526 U.S. 358, 373, 119 S. Ct. 1380, 1389, 143 L. Ed. 2d 462 (1999).
ERISA Long-Term Disability Cases
While most people are familiar with ERISA governing pension plans, 80% of all ERISA litigation is actually over denied long-term disability (LTD) benefits.
- What is the LTD benefit?
Employer-sponsored LTD plans, also known as “group” disability insurance plans, generally provide benefits after 6 months of disability until retirement age. The benefit is typically 2/3 of pre-disability earnings. Unlike private disability plans, almost all ERISA LTD plans will offset other income or benefits including severance, workers’ compensation, Social Security Disability, state disability, and even retirement benefits received. TIP: if you are negotiating a settlement for your client, be sure that it cannot be characterized as an off-settable source of income to the ERISA LTD benefits, or the client will essentially have to hand over the settlement funds to the ERISA LTD insurer.
Example of a severance that will likely be offset 100%: “After the Separation Date, EMPLOYEE will receive payments from EMPLOYER totaling $65,000, constituting salary continuation, accumulated sick leave, lost wages, and severance pay.”
Example of a severance that will not likely be offset: “After the Separation Date, EMPLOYEE will receive payments from EMPLOYER totaling $65,000 as consideration for waiving the claims specified herein. This amount does not constitute salary continuation, accumulated sick leave, lost wages, or severance pay.”
If it is impossible to avoid the triggering language, just leave out the description as a last resort.
- When Is Someone Disabled?
Many ERISA LTD plans have an “own occupation” standard of disability that shifts to an “any occupation” standard of disability after 24 months. In other words, after 24 months, the claimant has to be disabled from any occupation given her education, training, experience, and station in life, to continue to receive LTD benefits.
Many ERISA LTD plans also have a 2-year limitation for certain conditions. Common limitations include mental illnesses, “self-reported” conditions, neuro-musculoskeletal disorders, chronic fatigue conditions, chronic pain conditions, allergies, and chemical sensitivities. TIP: if you are working with a disabled client’s physicians and there are also emotional distress issues, be aware that the mental health component should be listed as secondary to the physical component of the disability to avoid the 24-month mental health limitation in the ERISA LTD plan.
Types of Plans
There are two types of ERISA LTD Plans: insured and self-funded. With self-funded plans, the employer sets aside funds for qualified participants. Because the risk of payment lies with the employer, usually big employers like AT&T or Johnson & Johnson are the only employers providing self-funded plans. With these plans, non-preempted state law insurance protections do not apply. With insured plans, the employer purchases an insurance policy to provide disability benefits to its. Often, the insurer both decides liability and pays the benefits. The Supreme Court recognizes this as a structural conflict of interest. Metropolitan Life Ins. Co. v. Glenn, 128 S. Ct. 2343 (2008). In my experience, some insurers are better than others. Standard Insurance currently has the worst definition of disability, limiting so many conditions to 24 months that it shocks me when someone is eligible for benefits beyond two years; Liberty Mutual is particularly cantankerous in litigation.
POP QUIZ!
Time for some ERISA issue spotting!
1. If someone has a disability or other employee benefit claim, does ERISA govern if the employer is:
A: A private company?
B: Government (U.C., federal employee, state employee, public school teacher)?
C: A partnership that covers both partners and employees?
D: A private company where there are only owners but no employees?
Answers: A: Yes; B: No; C: Yes; D: No (there must be an employee covered as well for ERISA to govern)
2. If someone has been disabled from her “own occupation” for 24 months, then the plan switches to an “any occupation” standard of disability, is she still entitled to benefits where she is:
A: a lawyer with bipolar disorder who is told by the insurer to go get a job as a manual laborer?
B: a construction worker who has a high school education but who also has lifting restrictions, where the insurer tells her to go get a job as a receptionist for a construction company?
Answers: A: No (not appropriate given education, training, experience, and station in life); B: Yes (as long as the salary matches her station in life)
3. What allegations will be preempted by ERISA?
A. Discrimination caused the employee to lose accrual of retirement benefits.
B. Emotional distress resulted from denied disability claim.
C. Employee was not paid fair wages.
D. California’s “notice prejudice” rule trumps an ERISA Plan’s claim filing deadline.
Answers:
A: Preempted – remedy of restored retirement conflicts with ERISA’s remedy for a breach of fiduciary duty claim. Ingersoll-Rand Co. v McClendon, 498 U.S. 478, 483 (1990);
B: Probably preempted: one court has recently held that emotional distress claims, if they are independent from the lost benefit claims, can proceed in state court. Daie v. The Reed Grp., Ltd., No. C 15-03813 WHA, 2015 WL 6954915, at *3 (N.D. Cal. Nov. 10, 2015) (“Our defendants’ duty not to engage in the alleged tortious conduct existed independent of defendants’ duties under the ERISA plan.”);
C: Not preempted: California Div. of Labor Standards Enf’t v. Dillingham Const., N.A., Inc., 519 U.S. 316, 328, 334 (1997);
D: UNUM Life Ins. Co. of Am. v. Ward, 526 U.S. 358, 373, 119 S. Ct. 1380, 1389, 143 L. Ed. 2d 462 (1999).
A Final Tip: Don’t Waive Your Client’s ERISA Claims in a Severance Agreement
Finally, many clients call me after having accepted a “standard” severance agreement from their employer, where they unknowingly waived their ERISA disability claim rights. Oops! While ERISA pension claims vest and cannot be waived, the same is not true for ERISA health and welfare claims, including disability claims. Please be sure that your clients do not waive their ERISA rights, as their disability and life insurance plans in particular may be far more valuable to them than the severance itself. Employers are generally willing to agree to carve out ERISA disability and life insurance claims once they understand the ramifications.
Example of a good ERISA carve-out: … However, the following claims are specifically and expressly excluded from the foregoing Release: (i) health insurance benefits under the Consolidated Omnibus Budget Reconciliation Act (COBRA); (ii) claims with respect to benefits, including short- and long-term disability benefit benefits, under a welfare benefit plan governed by the Employee Retirement Income Security Act (ERISA); or (iii) claims with respect to vested benefits under a retirement plan governed by ERISA.
If you ever have a question about how to navigate ERISA’s tricky waters, call an experienced ERISA attorney. Us ERISA nerds are typically happy to field questions and co-counsel if you find yourself in over your head. I can be reached at cassie@benefitslaw.com if you have any questions. You can also find more information about ERISA on the Department of Labor’s Employee Benefits Security Administration (EBSA) website, at https://www.dol.gov/ebsa/.
Cassie Springer Ayeni is the President and Founder of Springer Ayeni, A Professional Law Corporation, in Oakland, CA, where she focuses on ERISA disability and life insurance cases. She can be reached at cassie@benefitslaw.com or www.benefitslaw.com
Read More
Can you get benefits when Lyme disease forces you out of your job?
By Cassie Springer Ayeni
It happens: You’ve been working with Lyme disease for years and stumbling along. Some days/months are better than others, but you’ve been determined to keep working in a career you love. But then, gradually, it all becomes too much. You’re not bouncing back as well. Even though you rest from the moment you get home until when you leave for work the next day, giving up social engagements, relying on others to pick up the kids, and getting take-out dinners more than you would like, you are still struggling to get through the workday.
You see your doctor and she tells you the time has come for you to take some time off of work and focus on getting better. You are disabled from working. Now what? How will you live without your income? Here are some options and a plan.
- There Are Several Sources for Disability Benefits
Besides savings (and it is almost unheard of for someone in the prime of her working life to have sufficient savings to live decently for the rest of her days), income sources for people with disabilities include:
- ERISA-governed employee benefit plans (short-term disability then long-term disability). Long-term disability usually starts after 6 months and can last until retirement age.
- These benefits are usually tax-free if you paid the premiums with your after-tax earnings, but taxable if your employer paid the premiums.
- Private disability insurance plans (also lasting until retirement age).
- These benefits are usually not taxable.
- State disability insurance that usually last for a year (like California’s EDD).
- These benefits are usually not taxable.
- Social Security Disability Benefits (available after being disabled for six months and lasting through retirement age).
- These benefits are sometimes taxable, depending on your household income.
Here, I will focus on the first prong of these income sources: short- and long-term disability benefit plans offered by your employer. Many employers offer these group disability plans to all of their employees because the premiums are low and they can be a huge benefit to employees struck with a disability, whether short or long-term. Some employees never even realize that these benefits are in place, so be sure to check with HR or review your handbook as you are preparing to go out on disability.
However, a complex area of law called ERISA (the Employee Retirement Income Security Act) governs these employee benefit plans, even though you usually apply to an insurance company for payment of the benefits. Under ERISA, there are technical rules governing timelines for the insurance company to decide whether to pay your claim.
Even though you have a disability plan through your employer, you can still apply for all of the other disability benefits listed above. However, the benefits are usually coordinated so that you only receive a fixed percentage of your salary altogether, usually 2/3 or 60%.
- Your Doctor’s Role
Most people with Lyme disease have a long-standing relationship with a supportive doctor. This is instrumental to getting your disability benefit claims approved. Please make sure that your doctor knows how important it is that she fills out forms promptly so that your income stream can continue while you are not working. Here are some key tips for the “Attending Physician Statements” that you submit to the insurance company.
- Your doctor should answer the question “why is the patient disabled now?” especially if you have been working with Lyme disease for a while. Did it worsen? Is the fatigue getting the best of you? Is it now interfering with your ability to perform the activities of daily living, such as preparing meals? Ask your doctor to be specific and make sure this is in your medical record.
- Your doctor should point out that you are credible in your symptom reporting. When your doctor notes this, it helps prevent the insurance company from doubting your credibility, an unfortunately common reality when insurance companies are looking for a way to cut costs.
- Regularly schedule check-ups. Even though your condition may not get better with treatment, it is a good idea to see your doctor anyway every 6-12 months. This helps demonstrate to the insurance company that you are under the regular care of an attending physician. Also, insurance companies typically request medical records every 6-12 months.
- If you don’t already have an ERISA lawyer, you might want to check in with one now. Your lawyer can work with your doctor to get the forms filled out the right way the first time.
- Submitting the Application.
Finally, your doctor is on board and you have made the decision that resting without working is in the best interest of your health. Here is a checklist for your disability application:
- Request the short- and long-term disability application forms from HR.
- Request a copy of the short- and long-term disability policies from HR. These plan documents tell you some important information, like:
- The definition of disability. Make sure there is no “exclusion or limitation” for Lyme disease
- The Elimination Period. This tells you how long you have to be disabled before benefits start.
- The benefit amount. Typically this is 2/3 of your salary, when all sources of disability income are combined. There is often a “maximum” benefit, which high income earners need to be aware of.
- When the definition of disability “shifts.” Typically, for the first 24 months you are entitled to benefits if you are disabled from your regular occupation, and after 24 months you have to be disabled from “any occupation.”
- Duration of benefits. ERISA disability benefits usually last until retirement age or age 65, or until you are no longer disabled.
- The process for appealing a denied claim.
- Take a stab at filling out the application forms, but do not feel limited to the boxes on the forms. If you need extra space, include an addendum. If the question on the form doesn’t really apply to you, modify the question and answer to state what needs to be said about why you are disabled.
- Make sure that your employer knows they will have to fill out a form verifying your income and job duties.
- If it’s too overwhelming, ask an ERISA attorney to check your work to make sure that your application gives you the best shot at success. A skilled ERISA attorney will look for problems in your draft, and will also supplement an application with declarations and other information that will help an approval from the outset.
- And, if your application is denied, you must engage in the “appeals process” with the insurance company by the deadline, or you will lose your right to your claim. The appeal needs to contain ample medical and other evidence in support of your claim; it must be more than a letter stating “I appeal.” However, coming from someone who has handled hundreds of these appeals, you should never attempt to appeal on your own without the benefit of legal advice. The appeal stage is crucial, as you may be limited to the evidence of disability you present at this stage if you ever have to go to court.
Cassie Springer Ayeni is the President and Founder of Springer Ayeni, A Professional Law Corporation, in Oakland, CA, where she focuses on ERISA disability and life insurance cases. She can be reached at cassie@benefitslaw.com or www.benefitslaw.com.
Read More
