
Here’s a blast from the near past, which feels like a lifetime ago
So much has happened in these few months since I wrote this message to the Employee Benefits Committee as one of its incoming co-chairs. Since then, we had a successful midwinter meeting in Rancho Mirage, but none of us knew that would likely be our last travel occasion for the foreseeable future. Here’s a blast from the near past, which feels like a lifetime ago:
Read MoreLong Term Disability (LTD): The Hidden Gem in Your Benefits Package

What is an LTD benefit?
Most long-term disability benefits are insurance policies that provide about 50-67% of your base income should you become disabled. What does it mean to be disabled? It will be defined in the policy, but typically it is defined as the inability to perform the material duties of your occupation due to illness or injury. After some time, usually 24 months, the definition of “disability” may change to the inability to perform the material duties of any occupation (taking into account your education, training, and prior income level) due to illness or injury. Mental illness disabilities are usually limited to 24 months of benefits in total.
Many illnesses or injuries can qualify you for a disability benefit. Examples include back, neck, knee, or upper extremity pain, migraines, fibromyalgia, cancer and its consequences, HIV/AIDS, pulmonary dysfunction, cognitive impairment, neurological conditions like Parkinson’s Disease, or chronic pain conditions. Disabilities do not just strike the elderly; my clients range from ages 29-67, with most of them being in their 50s. Yet they all have one thing in common: none were expecting to have to stop working before retirement age due to a medical problem.
Who has an LTD benefit plan?
Most professionals work for employers that provide disability benefit plans. These disability insurance policies have relatively low premiums, so employers often provide disability insurance to their employees as a matter of course. If you work for an employer that provides professional, medical, or technology services you are a prime example of someone who probably has a disability benefit plan through your employer. For example, I frequently represent doctors, nurses, and other medical professionals, lawyers, engineers, project managers, programmers, financial services professionals, executive directors, and even insurance claims adjusters. To see if you have disability coverage, look up your original benefits package or examine what benefits you elected. You can also look up your employer’s IRS Form 5500 filing, which should include details on ERISA retirement and “welfare” benefits such as health, disability, and life insurance benefit plans. ERISA is the law that governs almost all employer-sponsored benefits.
What to do if you need to apply for LTD benefits?
If your doctor has advised you to stop working, please verify whether your employer has an LTD plan or give me a call and I’ll help you figure it out. There are other benefits that might be available to you as well (state disability, Social Security, workers’ compensation, etc.), which I can outline for you. If your employer does have an LTD plan, bear in mind that the reason you stop working has to be because of your disability for you to have coverage and make a successful LTD claim. In some states, including California, late applications can still be accepted as long as the insurer is not harmed by your late claim notice. Typically, your last date of work is also your first date of disability. If you are laid off for performance reasons that are actually related to your disability, you may still have a good LTD claim, but call me to help you analyze it. (You may also have a disability discrimination claim.) If you 1) have an employer-sponsored LTD plan, 2) need to stop working because of a medical condition, and 3) your doctor has advised you to stop working and will fill out a form on your behalf, you should strongly consider applying for LTD benefits. These benefits may be available until age 65 or 67, so do not shy away from making an application! However, there are many traps along the road of applying for and receiving LTD insurance benefits, so feel free to reach out to me if you have any questions about whether you should apply or how to maximize your chances of receiving benefits.

#LTD benefits
My Patient Needs to Stop Work … Now What?
By Cassie Springer Ayeni, Disability and Life Insurance Benefits Lawyer
with Springer Ayeni, A Professional Law Corporation
cassie@benefitslaw.com . www.benefitslaw.com
It happens: your patient comes to an appointment, and after months or years of “getting by” at work, despite a degenerative or chronic condition, it is clear to you that those days are over. You recommend that for her health, she stop working. Now what?
What your patient now faces is a host of forms and requests from insurance companies and the government to ensure that she has some income even though she’s not working anymore. Besides savings (and it is unheard of for someone in the prime of her working life to have sufficient savings to live decently for the rest of her days), income sources for people with disabilities include:
- Employee benefit plans (short-term disability then long-term disability). Long-term disability usually starts after 6 months and can last until retirement age.
- Private disability insurance plans (also lasting until retirement age).
- State disability insurance that usually last for a year (like California’s EDD).
- Social Security Disability Benefits (available after being disabled for a year and lasting through retirement age).
To qualify for any of these benefits, the #1 thing that a patient needs is help and support from the doctor. Without it, she won’t be approved; and if support wanes in the future, the insurance companies won’t hesitate to cut off her benefits. Here’s what you can do to help ensure that your patient receives disability benefit income on time and without hiccups:
Medical Records
- Document the reason why the patient is disabled in the medical records. List as many objective findings as are available (ROM, atrophy, MRIs, visual findings, etc.), including your objective observations.
- Document in the medical records whether the patient’s complaints of pain, fatigue, or other disabling symptoms are credible.
- If the patient has worked with the condition, answer the question in the medical records of “why now?” Why was she able to work before with the condition but suddenly cannot? Has there been a worsening of symptoms? Do you feel that her best chance of getting better is by resting for a bit at home? Document your rationale in the medical records.
- When the patient gets approved for benefits, keep track of the symptoms in regularly scheduled check-ups; insurance companies request updated medical records every 6-12 months.
Forms Requests
- Be sure to complete and return forms as quickly as possible. Although it is tempting to punt the form-filling to a secretary, it is more credible when completed by you.
- If there are any boxes on the forms that not applicable to your patient, just write N/A or rephrase the question so it makes sense for your patient
- Beware of traps in the questions: If a question states “how often can your patient work? 3 hours, 6, hours, or 8 hours a day,” but you feel your patient could only work 1 hour a day with breaks and unreliable, don’t check a box; just write your true response.
Working with the Lawyers
- Thankfully, with the increasing popularity of medical-legal alliances, most physicians and lawyers now truly comprehend their shared interest in the patient’s well-being, and working together on the insurance requests helps for seamless communications with the insurer. A patient about to go on disability can benefit from a quick call to a benefits attorney to make sure that every “I” is dotted and “t” is crossed.
- A patient whose disability benefits claim has been denied should never attempt to appeal on her own without the benefit of some legal advice.
- Also, even when a patient is approved for benefits, don’t hesitate to ask her lawyer for help understanding the forms; the lawyer and the patient will appreciate it more than you know.
Cassie Springer Ayeni is the President and Founder of Springer Ayeni, A Professional Law Corporation, in Oakland, CA, where she focuses on ERISA disability and life insurance cases. She can be reached atcassie@benefitslaw.com or www.benefitslaw.com
Read More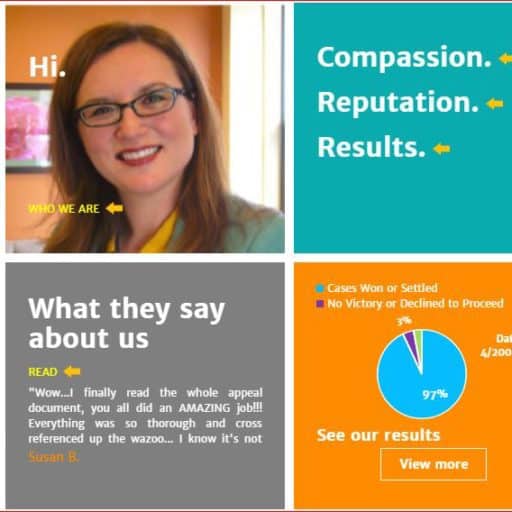
Know Disability Benefits Before Accepting A Job Offer
You found it: the perfect job for your next career move with a great salary. You are ready to give your acceptance! But before you do, understand what’s really included in the “benefits package” that your future employer described to you in broad strokes. Yes, there is health insurance and 401(k) matching, but an often-overlooked benefit that becomes crucial in a time of need is your employer’s long-term disability insurance benefit.
Many employers provide a long-term disability insurance policy to employees, which most employees could care less about because no one intends to be taken out of their profession by a disability. Yet a disability can come in many forms, and there are visible and invisible disabilities. You may be entitled to a disability benefit because you are recovering from a surgery, because you experience pain, because you have a degenerative condition, because you suffer from a brain injury, because you have a life-threatening condition, or due to mental health issues. Although you hope to never need to make a disability claim, it’s smart to be aware of what the plans provide should you need to make a short- or long-term disability claim.
The finances:
Disability insurance plans typically cover 60-66.67% of your base income. In general, if you pay the premiums with after-tax dollars as a payroll deduction, then the benefit is non-taxable. If your employer pays the premiums, then the benefit is taxable. Therefore, if you have the option, CHOOSE TO PAY THE PREMIUMS YOURSELF! The tax savings should you become disabled will be well-worth the monthly premium cost.
Disability insurance benefits typically pay through Social Security Normal Retirement Age, which is age 67 for those born in 1960 and later. A monthly income for the years when you are unexpectedly taken out of the workforce, particularly if your disability is expected to last for the rest of your life, is wonderful peace of mind.
Most disability insurance policies, however, cap the “maximum benefit” payable to a certain dollar amount per month. The lowest cap I’ve seen is $6,000 per month. The highest cap I’ve seen is $30,000 per month. If your plan has a low cap that would not be enough to sustain your quality of life if you become disabled, either reconsider the job offer or take our private disability insurance. You may even use this need for private insurance as a bargaining chip to negotiate for a higher salary, as such insurance is typically quite expensive.
The logistics:
Just because a disability benefit plan is offered, does not mean that approval for benefits under that insurance plan will be a piece of cake. If you have a disability that is degenerative in nature, take some time to plan your exit strategy over several months with your doctor’s advice. Work until your physician advises that you no longer should, and then seek the advice of an experienced ERISA attorney to guide you through the application process to ensure the best chance of success at the outset.
With some basic knowledge and the right planning, ERISA disability insurance benefits can be a valuable addition to your compensation package.
Cassie Springer Ayeni is the President of Springer Ayeni, A Professional Law Corporation, where she represents individuals in disability benefit applications, appeals, and lawsuits. She can be reached at www.benefitslaw.com
For more contact: Cassie Springer Ayeni
Read More
Reforming Disability Claim Procedures Under ERISA
On Dec. 19, 2016, the U.S. Department of Labor published in the Federal Register sweeping reforms to the regulations it issues under Section 503 of the Employee Retirement Income Security Act, aimed at eliminating bias in the ERISA disability claims and review process.
Despite ERISA’s reputation as an erudite law affecting primarily pension plans, the DOL reports that, “An empirical study of ERISA employee benefits litigation from 2006 to 2010 concluded that cases involving long-term disability claims accounted for 64.5 percent of benefits litigation whereas lawsuits involving health care plans and pension plans accounted for only 14.4 percent and 9.3 percent, respectively.” (p. 3.) Hence the DOL’s decision to take aim at the regulations affecting disability plan administration, which is typically handled by insurance carriers.
The DOL noted “the economic incentive for insurance companies to deny otherwise valid claims and because plans are often able to secure a deferential standard of review in court.” (p. 8.) Although the DOL received commentary that disability claims administrators should not be subject to the same rigorous regulations issued under the Affordable Care Act to health plan administrators, “the department views enhancements in procedural safeguards and protections similar to those required for group health plans under the Affordable Care Act as being just as important, if not more important, in the case of claims for disability benefits.” (p. 10.) It noted the need for transparency and accountability in all claims handling. (p. 11.)
The department enhanced protections for disability plan participants in eight ways (pp. 11-12):
Increased independence and impartiality of the decision makers
Adverse decisions must fully explain the reasons for the denials and why evidence of the claimant was disagreed with
Notification to claimants of the right to obtain their claim file and other documents before a final decision is made and to present testimony and other evidence in support of their claim
Provision of an opportunity for claimants to respond to adverse medical opinions before a final decision is made
A guarantee that a claimant can proceed to litigation if the administrator fails to comply with the DOL regulations (stricter than “substantial compliance”)
A guarantee that a rescission of coverage triggers appeal rights under the regulations
Cultural and linguistically appropriate requirements for communications
A requirement that the notice of an adverse benefit determination on review must include a description of any applicable contractual limitations period and its expiration date (p. 54)
But perhaps the biggest protection is the first, requiring impartiality not just in claims decision makers, but also in vocational experts, medical consultants and in-house medical reviewers. (pp. 13-15.) And the DOL understood and took issue with the notion that impartiality could be achieved if the administrator, for example, hires a company who then hires the medical expert for review. It stated: “The text of the rule does not limit its scope to individuals that the plan directly hires. Rather, the rule’s coverage extends to individuals hired or compensated by third parties engaged by the plan with respect to claims.” (p. 15.) It cautioned that such a prohibition should not temper a court’s inquiry into the neutrality of the expert, noting the availability of discovery to probe such matters. (p. 16.)
The DOL further disabused the insurance practice of rejecting experts that would support an approval of benefits in favor or experts that would support denial as inappropriate “expert shopping.” (p. 20.) It found that “[r]equiring plans to explain the basis for disagreeing with experts whose advice the plan sought” should help that problem. (p. 20.) The department couched the requirement to explain disagreement with medical and vocational professionals in denying a claim “as a matter of basic fiduciary accountability.” (p. 22.)
Regarding Social Security disability awards, the department was careful to specify that although it does not expect administrators to defer to a favorable Social Security disability determination, “a more detailed justification would be required in a case where the U.S. Social Security Administration definitions were functionally equivalent to those under the plan.” (p. 25.) It refused, however, to adopt the “treating physician rule” present in Social Security decisions, where the administrator must defer to the opinion of the treating physician. (p. 25.)
The department vigorously defended its decision to allow claimants to review and rebut evidence that would be used to deny a claim. Commenters argued that claimants could provide an endless loop of evidence supporting a claim that the administrator would have to rebut endlessly as well. The DOL dismissed that argument as contrary to fiduciary obligations: “The fiduciary obligation to pay benefits in accordance with the terms of the plan does not require a fiduciary to endlessly rebut credible evidence supplied by a claimant that, if accepted, would be sufficient to justify granting the claim. In fact, an aggressive claims-processing practice of routinely rejecting or seeking to undermine credible evidence supplied by a claimant raises questions about whether a fiduciary, especially one operating under a conflict of interest, is violating the fiduciary’s loyalty obligation under ERISA to act solely in the interest of the plan’s participants and beneficiaries.” (p. 37.)
Controversially, the department approved a “tolling” of timelines for responding to claims and appeals where the claimant submits additional evidence for the administrator to consider. “In the department’s view, the current disability claims regulation ‘special circumstances’ provision permits the extension and tolling expressly added to the group health plan rule under the ACA claims and appeals final rule.” (p. 40.) It remains to be seen if this will deny claimants swift access to the courts or even allow a statute of limitations to expire while tolling is in place. See Heimeshoff v. Hartford Life & Accident Insurance Co., 134 S.Ct. 604, 611 (2013). Perhaps in anticipation of this conundrum, the department addressed the potential problem raised by the Heimeshoff decision where a statute of limitations could expire while a participant was engaging in the mandatory review process prescribed under ERISA Section 503. It stated:
First, Section 503 of ERISA requires that a plan afford a reasonable opportunity to any participant whose claim for benefits has been denied for a full and fair review of that decision by 53 an appropriate named fiduciary. The department does not believe that a claims procedure would satisfy the statutory requirement if the plan included a contractual limitations period that expired before the review was concluded …
A limitations period that expires before the conclusion of the plan’s internal appeals process on its face violates ERISA Section 503’s requirement of a full and fair review process. A process that effectively requires the claimant to forego the right to judicial review and thereby insulates the administrator from impartial judicial review falls far short of the statutory fairness standard and undermines the claims administrator’s incentives to decide claims correctly. (pp. 52-53.)
It further stated that a contractual limitations period that does not permit a lawsuit after the conclusion of an administrative appeal “is unenforceable.” (pp. 53-54.) In an effort to provide transparency, the department will now require administrators to state any contractual limitations period “including the date by which the claimant must bring a lawsuit” in a final adverse decision. (p. 53.)
However, the department did not provide much leeway for plan administrators to avoid litigation for failing to comply with the regulations. In fact, for the administrator to argue failure to exhaust administrative remedies despite noncompliance, the administrator’s failure to comply must be all of the following: “(1) de minimis; (2) nonprejudicial; (3) attributable to good cause or matters beyond the plan’s control; (4) in the context of an ongoing good-faith exchange of information; and (5) not reflective of a pattern or practice of noncompliance.” (p. 42.)
The department refused to provide a general rule on the level of deference an administrator would receive from a reviewing court, but did indicate that where the administrator’s noncompliance has resulted in a claim’s deemed exhaustion, the “legal effect of the definition may be that a court would conclude that de novo review is appropriate because of the regulation that determines as a matter of law that no fiduciary discretion was exercised in denying the claim.” (pp. 43-44.)
Read More

PRACTICE GUIDE: ERISA ISSUE SPOTTING – HOW TO AVOID MALPRACTICE
ERISA. The acronym strikes terror in the heart of many a lawyer. Fuzzy notions of fiduciary duties, equitable remedies in the days of a divided bench, and preemption can cause even the most erudite of attorneys to break into a cold sweat. My friends: speaking as someone who has handled ERISA claims, litigation, and appeals for 15 years, I’m here to tell you that it is really not that bad! Allow me to walk you through some ERISA basics so that you can issue spot and avoid malpractice.
ERISA Fundamentals
The Employee Retirement Income Security Act of 1974 (ERISA) provides minimum standards for voluntarily established benefit plans in the private industry. In addition to pension plans, ERISA governs health and welfare benefit plans, including employer-sponsored disability and life insurance plans. ERISA does not cover benefit plans established or maintained by governmental entities, churches for their employees, or plans which are maintained solely to comply with applicable workers compensation, unemployment, or disability laws. This means that UC plans are non-ERISA (government) plans, but an employer’s benefit plans are governed by ERISA.
ERISA requires plans to provide participants with plan information. ERISA § 104(b)(4). Those who manage and control plan assets must act as fiduciaries. ERISA § 404. ERISA plans must have a grievance and appeals process for benefit claims. ERISA § 503. The process of appealing a denied benefit claim is also called a “request for review,” and is crucial to achieving success on a denied benefit claim, either with the administrator or before a federal court. TIP: There is a 180-day deadline for submitting ERISA appeals that CANNOT be missed. Finally, ERISA gives participants and beneficiaries the right to sue for benefits and breaches of fiduciary duty. ERISA § 502(a). Lawsuits related to or remedied by ERISA are brought in federal district court. Statutes of limitations are often identified in the ERISA plans themselves and must be adhered to.
ERISA Preemption
ERISA has broad preemption provisions. ERISA § 514. If a remedy is available under ERISA, the claim will be preempted. If a case “relates to” an ERISA plan because there is a “connection with or reference to” a plan, the case will be preempted. Metro. Life Ins. Co. v. Massachusetts, 471 U.S. 724, 739. For example, in Ingersoll-Rand Co. v McClendon, the Supreme Court held that a wrongful discharge action was preempted by ERISA because the plaintiff alleged that the wrongful termination was primarily because of the employer’s desire “to avoid contributing to, or paying benefits under, the employee’s pension fund.” 498 U.S. 478, 483 (1990). However, in another case, the Supreme Court determined that California’s prevailing wage law is not preempted by ERISA because the law does not “make reference to” ERISA plans, nor does it have a connection to an ERISA plan because “[t]he prevailing wage statute alters the incentives, but does not dictate the choices, facing ERISA plans.” California Div. of Labor Standards Enf’t v. Dillingham Const., N.A., Inc., 519 U.S. 316, 328, 334 (1997).
As a general rule, if the alleged harm is that the unlawful conduct interfered with a right to receive, vest in, or accrue an employee benefit, then the claim will be preempted. Ingersoll-Rand Co. v. McClendon, 498 U.S. 133 (1990) (preempting a common law wrongful discharge claim where the claim was that the employer retaliated to prevent vesting in an ERISA plan). TIP: If you are concerned that your case will be pre-empted by ERISA, avoid alleging that any remedies are available under any kind of employee benefit plan or that any claims bear a connection to an employee benefit plan. Do NOT allege that the bad behavior caused a loss of employee benefits. Do NOT allege that the bad behavior should result in payment of disability or other ERISA benefits. These allegations will cause you to be removed to the federal courts that have exclusive jurisdiction over ERISA claims. And, if the claim is properly an ERISA claim for benefits, then there will be no consequential or punitive damages available, nor will there be a jury trial.
However, ERISA’s “savings clause” provision saves from preemption any law that regulates insurance, banking, or securities. ERISA § 514(b)(2)(A). An example of the application of the savings clause is in California’s “notice prejudice” rule, which provides that claims can proceed even where there is late notice unless the insurer is prejudiced by the late notice. Because this is a law that regulates insurance and does not provide a remedy that conflicts with ERISA, the law is not preempted. UNUM Life Ins. Co. of Am. v. Ward, 526 U.S. 358, 373, 119 S. Ct. 1380, 1389, 143 L. Ed. 2d 462 (1999).
ERISA Long-Term Disability Cases
While most people are familiar with ERISA governing pension plans, 80% of all ERISA litigation is actually over denied long-term disability (LTD) benefits.
- What is the LTD benefit?
Employer-sponsored LTD plans, also known as “group” disability insurance plans, generally provide benefits after 6 months of disability until retirement age. The benefit is typically 2/3 of pre-disability earnings. Unlike private disability plans, almost all ERISA LTD plans will offset other income or benefits including severance, workers’ compensation, Social Security Disability, state disability, and even retirement benefits received. TIP: if you are negotiating a settlement for your client, be sure that it cannot be characterized as an off-settable source of income to the ERISA LTD benefits, or the client will essentially have to hand over the settlement funds to the ERISA LTD insurer.
Example of a severance that will likely be offset 100%: “After the Separation Date, EMPLOYEE will receive payments from EMPLOYER totaling $65,000, constituting salary continuation, accumulated sick leave, lost wages, and severance pay.”
Example of a severance that will not likely be offset: “After the Separation Date, EMPLOYEE will receive payments from EMPLOYER totaling $65,000 as consideration for waiving the claims specified herein. This amount does not constitute salary continuation, accumulated sick leave, lost wages, or severance pay.”
If it is impossible to avoid the triggering language, just leave out the description as a last resort.
- When Is Someone Disabled?
Many ERISA LTD plans have an “own occupation” standard of disability that shifts to an “any occupation” standard of disability after 24 months. In other words, after 24 months, the claimant has to be disabled from any occupation given her education, training, experience, and station in life, to continue to receive LTD benefits.
Many ERISA LTD plans also have a 2-year limitation for certain conditions. Common limitations include mental illnesses, “self-reported” conditions, neuro-musculoskeletal disorders, chronic fatigue conditions, chronic pain conditions, allergies, and chemical sensitivities. TIP: if you are working with a disabled client’s physicians and there are also emotional distress issues, be aware that the mental health component should be listed as secondary to the physical component of the disability to avoid the 24-month mental health limitation in the ERISA LTD plan.
Types of Plans
There are two types of ERISA LTD Plans: insured and self-funded. With self-funded plans, the employer sets aside funds for qualified participants. Because the risk of payment lies with the employer, usually big employers like AT&T or Johnson & Johnson are the only employers providing self-funded plans. With these plans, non-preempted state law insurance protections do not apply. With insured plans, the employer purchases an insurance policy to provide disability benefits to its. Often, the insurer both decides liability and pays the benefits. The Supreme Court recognizes this as a structural conflict of interest. Metropolitan Life Ins. Co. v. Glenn, 128 S. Ct. 2343 (2008). In my experience, some insurers are better than others. Standard Insurance currently has the worst definition of disability, limiting so many conditions to 24 months that it shocks me when someone is eligible for benefits beyond two years; Liberty Mutual is particularly cantankerous in litigation.
POP QUIZ!
Time for some ERISA issue spotting!
1. If someone has a disability or other employee benefit claim, does ERISA govern if the employer is:
A: A private company?
B: Government (U.C., federal employee, state employee, public school teacher)?
C: A partnership that covers both partners and employees?
D: A private company where there are only owners but no employees?
Answers: A: Yes; B: No; C: Yes; D: No (there must be an employee covered as well for ERISA to govern)
2. If someone has been disabled from her “own occupation” for 24 months, then the plan switches to an “any occupation” standard of disability, is she still entitled to benefits where she is:
A: a lawyer with bipolar disorder who is told by the insurer to go get a job as a manual laborer?
B: a construction worker who has a high school education but who also has lifting restrictions, where the insurer tells her to go get a job as a receptionist for a construction company?
Answers: A: No (not appropriate given education, training, experience, and station in life); B: Yes (as long as the salary matches her station in life)
3. What allegations will be preempted by ERISA?
A. Discrimination caused the employee to lose accrual of retirement benefits.
B. Emotional distress resulted from denied disability claim.
C. Employee was not paid fair wages.
D. California’s “notice prejudice” rule trumps an ERISA Plan’s claim filing deadline.
Answers:
A: Preempted – remedy of restored retirement conflicts with ERISA’s remedy for a breach of fiduciary duty claim. Ingersoll-Rand Co. v McClendon, 498 U.S. 478, 483 (1990);
B: Probably preempted: one court has recently held that emotional distress claims, if they are independent from the lost benefit claims, can proceed in state court. Daie v. The Reed Grp., Ltd., No. C 15-03813 WHA, 2015 WL 6954915, at *3 (N.D. Cal. Nov. 10, 2015) (“Our defendants’ duty not to engage in the alleged tortious conduct existed independent of defendants’ duties under the ERISA plan.”);
C: Not preempted: California Div. of Labor Standards Enf’t v. Dillingham Const., N.A., Inc., 519 U.S. 316, 328, 334 (1997);
D: UNUM Life Ins. Co. of Am. v. Ward, 526 U.S. 358, 373, 119 S. Ct. 1380, 1389, 143 L. Ed. 2d 462 (1999).
A Final Tip: Don’t Waive Your Client’s ERISA Claims in a Severance Agreement
Finally, many clients call me after having accepted a “standard” severance agreement from their employer, where they unknowingly waived their ERISA disability claim rights. Oops! While ERISA pension claims vest and cannot be waived, the same is not true for ERISA health and welfare claims, including disability claims. Please be sure that your clients do not waive their ERISA rights, as their disability and life insurance plans in particular may be far more valuable to them than the severance itself. Employers are generally willing to agree to carve out ERISA disability and life insurance claims once they understand the ramifications.
Example of a good ERISA carve-out: … However, the following claims are specifically and expressly excluded from the foregoing Release: (i) health insurance benefits under the Consolidated Omnibus Budget Reconciliation Act (COBRA); (ii) claims with respect to benefits, including short- and long-term disability benefit benefits, under a welfare benefit plan governed by the Employee Retirement Income Security Act (ERISA); or (iii) claims with respect to vested benefits under a retirement plan governed by ERISA.
If you ever have a question about how to navigate ERISA’s tricky waters, call an experienced ERISA attorney. Us ERISA nerds are typically happy to field questions and co-counsel if you find yourself in over your head. I can be reached at cassie@benefitslaw.com if you have any questions. You can also find more information about ERISA on the Department of Labor’s Employee Benefits Security Administration (EBSA) website, at https://www.dol.gov/ebsa/.
Cassie Springer Ayeni is the President and Founder of Springer Ayeni, A Professional Law Corporation, in Oakland, CA, where she focuses on ERISA disability and life insurance cases. She can be reached at cassie@benefitslaw.com or www.benefitslaw.com
Read More




